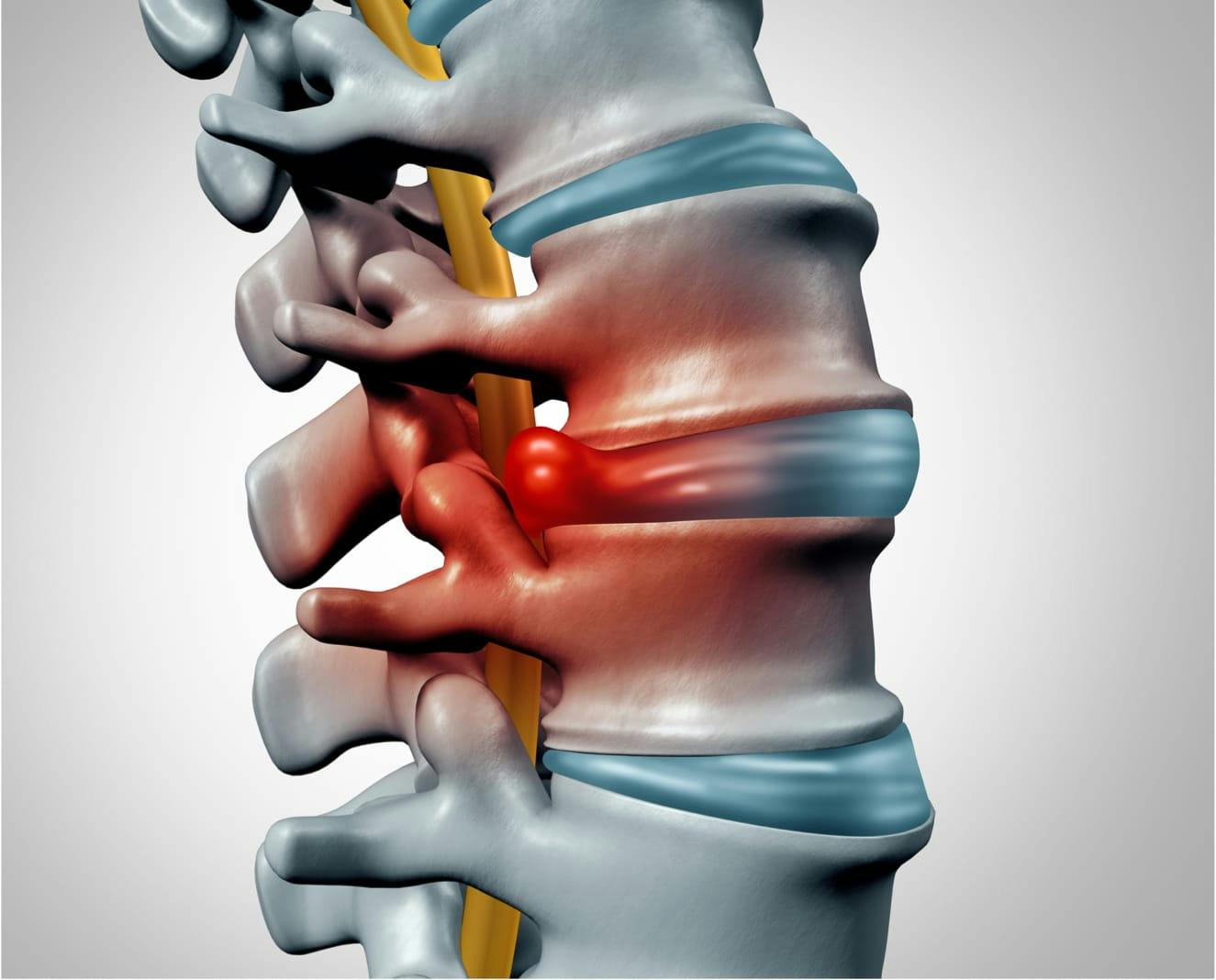
Dr. Jonathan Stieber is known throughout New York for his effective and personalized approach to resolving back pain. During your consultation, he will formulate a custom treatment plan that is based on your symptoms. Conservative approaches may be all that’s required if your condition is steadily improving. If your condition continues to worsen, Dr. Stieber's herniated disc surgery in NYC may be the best treatment option.
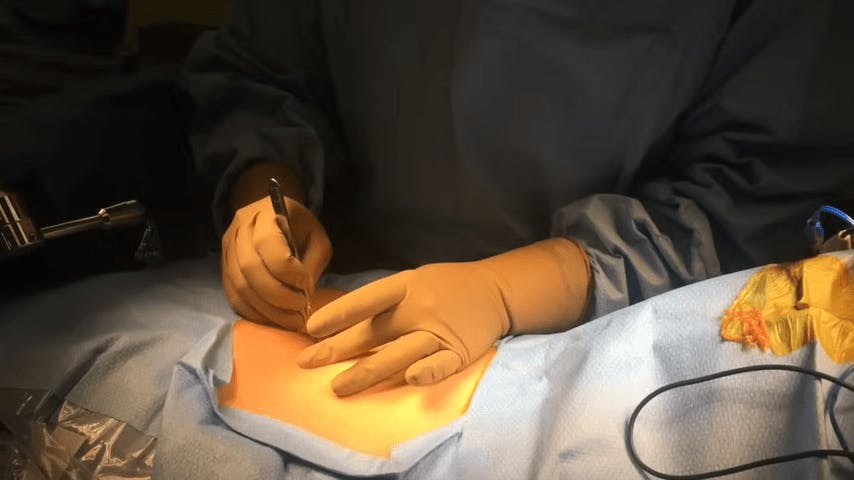
The standard surgical procedure for treatment of a lumbar herniated disc is laminotomy and discectomy. During the procedure, Dr. Stieber will remove a small piece of the bone to gain access to the spinal canal (laminotomy) and then removes a portion of the herniated disc (discectomy). Spinal fusion may be required in certain cases.
For lumbar disc herniation patients requiring herniated disc surgery, Dr. Stieber offers the most advanced minimally invasive treatment options using extremely small incisions and allowing outpatient treatment. During a tubular microdiscectomy, a robotic microscope will be used to remove the offending herniated disc through an incision of 16-18mm.
Endoscopic discectomy is a procedure that utilizes a specialized camera inserted into the spinal canal through a ¼ inch incision and dedicated instruments to treat damaged discs. Benefits of these minimally-invasive approaches include decreased pain, quicker recovery, and an enhanced cosmetic result.